Both alcohol and Xanax have their places in the lives of people all across the globe. Xanax (a brand name for alprazolam) is a prescription medication that belongs to the class of drugs known as benzodiazepine. Xanax is used to treat depression, panic disorders, and anxiety disorders, making life much more manageable for more than five percent adult population of the United States. Similarly, alcohol is a legal substance often found at social gatherings and at many dinner tables.
Although both substances can be healthy and safe on their own, mixing Xanax and alcohol can have devastating short-term and long-term effects, as can the combination of many prescription and illicit drugs with alcohol.
Unfortunately, it is pretty common for people to mix Xanax with alcohol. Here is what you need to know if you or someone you know is taking Xanax and alcohol or if you believe they are also mixing other drugs.
Mixing Xanax and Alcohol
When used within the therapeutic dose range, Xanax is generally regarded as safe. However, dangerous and sometimes fatal interactions can occur when an individual takes high doses of Xanax or use the Xanan with other addictive substances, such as alcohol.
Alcohol and Xanax both enhance the activity of the inhibitory neurotransmitter gamma-aminobutyric acid (GABA) and the overall activity of the central nervous system (CNS). This leads to a sedative effect. When both depressants are combined, it can result in respiratory depression, cardiac arrest, and loss of consciousness.
Drinking alcohol in larger amounts causes lethargy. Combining these substances has a synergistic effect. If you consume a large amount of Xanax with alcohol, you will likely experience euphoria. This heightened sense of calmness and reduced anxiety might lead to dual addiction.
Those who consume more alcohol than Xanax are likely to lose consciousness quickly; in rare cases, this can result in a coma.
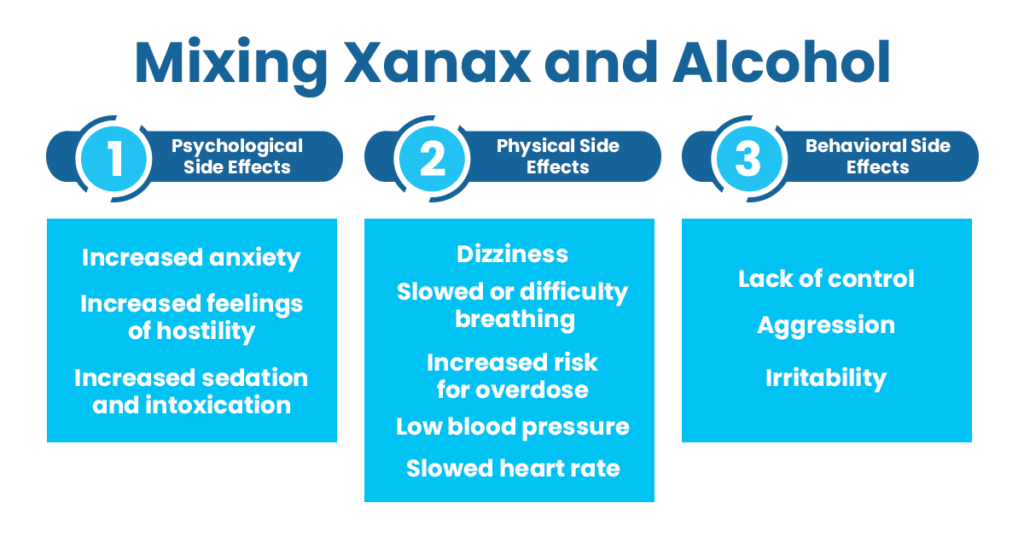
Common Side Effects of Mixing Xanax and Alcohol
Users should be aware of a number of signs and symptoms of concurrent Xanax and alcohol abuse. Abuse of Xanax can induce intense feelings of relaxation and even euphoria. These euphoric feelings serve as a positive reward for Xanax abuse and raise the likelihood of addiction. When Xanax is taken with alcohol, the effects of both substances get amplified.
Here are the physical, psychological, and behavioral effects of mixing Xanax and alcohol:
Physical Side Effects
- Dizziness
- Slowed or difficulty breathing
- Increased risk for overdose
- Low blood pressure
- Slowed heart rate
- Coma
- Unusual behavior
- Liver damage
- Impaired motor skills
- Drowsiness
- Memory problems
- Death
Psychological Side Effects
- Increased anxiety
- Increased feelings of hostility
- Increased sedation and intoxication
Behavioral Side Effects
- Lack of control
- Aggression
- Irritability
What makes the mixture of alcohol and Xanax so deadly is that it’s hard to tell when you’ve had too much. A person can swiftly go from feeling somewhat drugged to extremely intoxicated. Your body requires time to process these substances. During this time, it is easy to consume too much without recognizing it.
Xanax should never be used with alcohol for medical purposes; it should always be taken as prescribed. This implies that no amount of alcohol is deemed safe when taking Xanax. Some individuals may take Xanax with alcohol and have no serious side effects.
Who is at a Higher Risk to Be Affected by Alcohol and Xanax?
Usually, women are at higher risk than men for the negative consequences of substance use disorders (SUDs). Women contain less water in their bodies than men do. This indicates that the quantity of alcohol consumed gets more concentrated when combined with water in the body, resulting in a greater blood alcohol concentration. When women combine Xanax and alcohol, the effects might be more acute.
Old people are specifically at a higher risk. The body’s capacity to metabolize alcohol decreases with age. Therefore, alcohol remains in the system longer. Additionally, this age group is often prescribed medications. If Xanax is a regular prescription, combining it with alcohol can significantly increase its negative side effects.
College students are more prone to abuse benzodiazepines like Xanax. Between 1993 and 2005, the number of students in the United States who used these drugs climbed by 450 percent. Because Xanax has been characterized as a medication with low abuse potential and minimal dependency risk, it has been classed as a schedule IV substance. This leads people to believe that it is safer to take than marijuana, a schedule I drug. This comparison undoubtedly contributed to the increased recreational usage of Xanax.
In addition to its drug categorization, the normalization of Xanax among college students is heavily influenced by the effects of friendship and peer pressure on the brain. At this age, young people stop relying on their parents and instead prioritize their friendships. Friendships can directly impact the decisions of young people. Teenagers are more willing to take risks with their friends than they would be alone. This is because taking risks and getting acceptance from friends stimulates the reward center of the brain.
Treatment for Alcohol and Xanax Addiction
The first step in the treatment of any addiction is reaching out to a treatment facility (or addict expert) in order to locate the right treatment program. The most critical step after calling an addiction treatment center is arranging an assessment or substance abuse examination to identify the degree of the addiction. After that, the proper level of care for the patient will then be determined.
When dealing with benzodiazepine addiction, medical attention and supervision are required regardless of the circumstances. It is essential to remain patient during the treatment to achieve long-term recovery from a Xanax or alcohol addiction.
Medical detox helps reduces the likelihood of experiencing potentially harmful withdrawal symptoms. During the detox process, a team of medical specialists offers 24-hour care and medications to alleviate withdrawal symptoms.
It may be overwhelming to enter an inpatient treatment program, but it offers the highest chance of recovery. In addition to being continuously watched by a team of medical professionals, you will also get long-term care that will provide you with the tools to remain healthy and clean.
In addition to medical detox and inpatient, counseling and therapy sessions are crucial components of the treatment process. This enables former addicts to address the causes of their addiction and develop healthy coping skills for the future.
Frequently Asked Questions (FAQs)
Can you take Xanax 2 hours after drinking?
Alcohol has a half-life of 4–5 hours. This is how long it takes for your body to eliminate 50 percent of the alcohol from the body. The body takes four to five half-lives to eliminate 94 to 97 percent of alcohol. This indicates that the majority of alcohol should be eliminated from the body between 16 to 25 hours.
Therefore, it is not safe to take Xanax two hours after drinking.
Can you drink 4 hours after Xanax?
You may have taken Xanax and want to know how long you must wait before consuming alcohol. In healthy people, the average half-life of Xanax is 11.2 hours, with a range of 6.3–26.9 hours. The half-life is the time needed for half of the drug to be eliminated from the body. Approximately 4–5 half-lives are required to eliminate 94 to 97 percent of a drug from the body.
Although, on average, it takes 56 hours for a single dose of Xanax to be eliminated from the body, various factors (including age, liver function, and obesity) might impact how long Xanax stays in the body.
Therefore, it is not safe to drink four hours after taking Xanax.
What would happen if you took Xanax while drinking alcohol?
Both alcohol and Xanax have distinct side effects that affect a person’s behavior and mental state. Because of this, alcohol and Xanax should never be combined since doing so might result in life-threatening effects. When used with alcohol, Xanax can cause the heart to stop beating, interfere with neurological function, and decrease breathing to the point of respiratory failure, severe brain damage, coma, or even death. In addition, it raises the probability of a Xanax overdose, which can result in respiratory depression, seizures, and even death. Alcohol plus Xanax can relax and delay biological functioning to the point that the user stops breathing or their heart stops beating, resulting in a coma and death.
Is it okay to mix a small dose of Xanax with alcohol?
In short, the answer is “absolutely not.” Everyone has different alcohol and Xanax tolerance levels; hence, the term “small dose” is completely subjective and meaningless when tolerance is considered. Alcohol and Xanax both influence the GABA neurotransmitter system in the brain; however, many people do not recognize that some substances combination multiply their effects together. Even if your alcohol consumption is normal (i.e., you do not exceed your limit) and you combine Xanax with it, the cumulative effect is typically unexpected and oftentimes dangerous.
The Haven Detox Can Help You Overcome Addiction
Recovery is possible, but the first step is to seek help. There is no shame in admitting that you are struggling with an addiction problem and need help. Even though this step is sometimes terrifying to take, it is the first step toward a healthier, happier, and more fulfilling life in recovery.
If you or a loved one are mixing Xanax and alcohol, it is crucial to get treatment before the disease of addiction advances. At The Haven Detox, we provide a dual diagnosis treatment to assist you in overcoming your Xanax and alcohol addictions. Our team of doctors and healthcare providers offers treatment in the comfort of an inpatient environment, allowing you to focus entirely on your recovery without the hassles and expectations of daily life.
Contact us at (844) 933-4145 immediately if you are interested in learning more about our treatment programs. Even if you don’t know where to turn for help, we can assist you in dealing with the negative effects of alcohol, mental health problems, or prescription medications.